Baby Blues or Postpartum Depression? How to Figure Out What You Are Experiencing
How Long do The Baby Blues Last?
So you’ve recently had a baby and the emotions are setting in. Naturally, you’re feeling a lot of things and you might be wondering: “Am I experiencing the baby blues or postpartum depression?” Your life has changed drastically in a short amount of time and your body is also reacting. During pregnancy, your progesterone levels increase up to 200x their baseline levels and when you deliver your placenta, that progesterone is leaving the body causing a steep drop. Sounds a little bit like a roller coaster, right? So if you’re emotionally feeling like a roller coaster, this is probably why and you are not the only one.
How can you tell if what you are experiencing is a “natural” part of the transition of baby from inside to outside of your body and the drastic change in hormones that brings? How can you tell if you need to seek outside help or if this will subside on its own?
What Contributes to Postpartum Mental Wellness?
As mentioned above, there are natural swings in hormone levels when you are pregnant, during birth and after. Your body is changing along with the needs of a growing baby and the transition from inside the body to outside the body. Additionally, starting the process of breast milk production causes hormone fluctuation whether you decide to breastfeed or not. Late in pregnancy, many women struggle to sleep and when the baby arrives, many women experience ongoing sleep deprivation. This lack of sleep can make it harder for hormone levels and emotional responses to return to a baseline level as the brain and body do not experience restorative rest. This means it can take weeks and even months to stabilize.
What is Baby Blues?
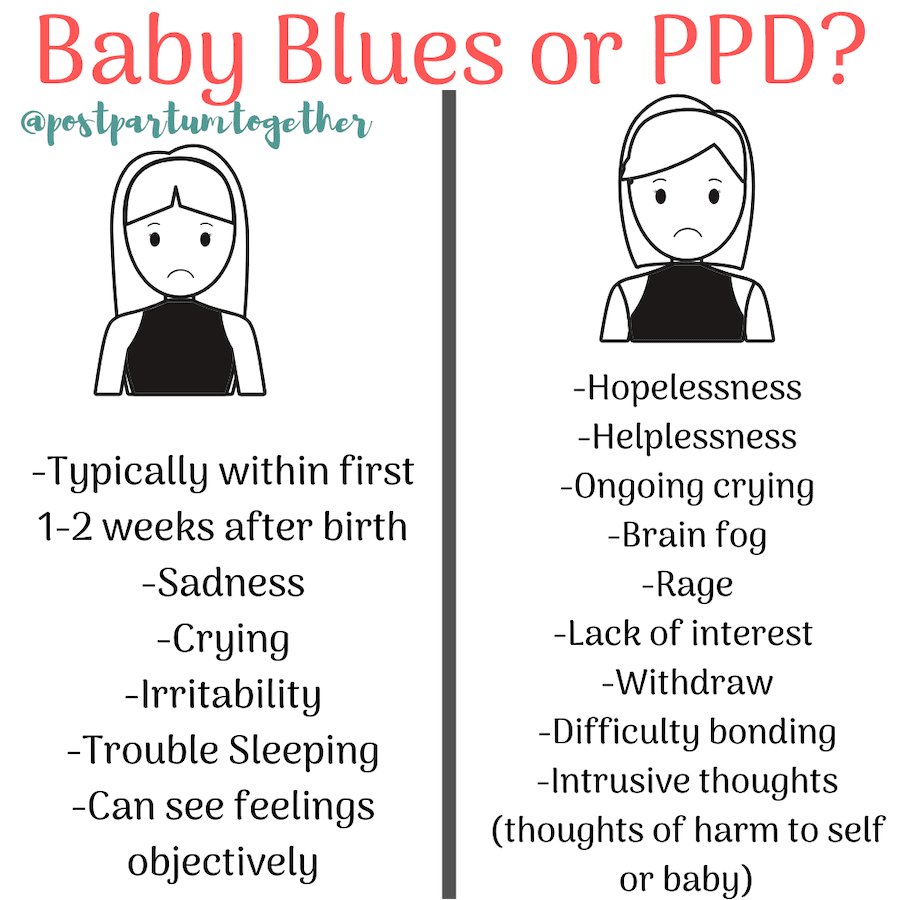
-Typically within first 1-2 weeks after birth
-Sadness
-Crying
-Irritability
-Trouble Sleeping
-Can see feelings objectively
With baby blues, women can identify that this is temporary and marked by things like lack of sleep, big transitions and hormone shifts. The mom with baby blues recognizes that this is difficult, but knows it will pass and can see things objectively. She feels these things but does not feel that they are all-consuming.
What is Postpartum Depression?
-Hopelessness
-Helplessness
-Ongoing crying
-Brain fog
-Rage
-Lack of interest in people or things
-Withdraw
-Difficulty bonding
-Intrusive thoughts (thoughts of harm to self or baby)
The mom who is experiencing postpartum depression will see symptoms beyond the first two weeks. Symptoms may onset after delivery to up to 1 year postpartum. This mom might feel that there is no end to the negative emotions. She feels withdrawn and not interested in people or things she was previously interested in. She may not be able to “find” or recognize herself in the midst of all of the emotions. This mom may have rage she cannot control. In some cases, this mom believes the baby would be better off without her and she struggles with intrusive thoughts of harm.
RELATED: Postpartum Depression and Anxiety Stories
PPD Risk Factors
While there are no guarantees about who will and who will not experience PPD, there are some risk factors that increase your likelihood.
Women who:
-Have a history of mental health disorders
-With a mother/father/grandparent/sibling with a history of a mental health disorder
-Pregnancy, birth, or postpartum medical complications-Mothers with baby in the NICU
-Mothers of baby with colic or medical complexity
-Women with little family/friend/community support
If you are pregnant and know that you are at risk for PPD, Burd Therapy’s Preventing PPD course may be the tool you need.
Everyone Deserves Postpartum Support
Whether you are struggling with baby blues, postpartum depression, or just going through the transition into motherhood, you deserve support and there is no shame in not having it “all together.” No one really has it all together, even if it appears that way on the outside. If you believe you may be struggling with PPD, contact your provider- either your OB or your Primary Care Provider, and tell her how you’re feeling. If possible, find a therapist who can provide you with a safe space to talk about your transition and feelings. Share your experience with those who are close to you and care about you- many people want to be helpful and supportive and there is no reward for doing it all yourself.
Whether it is medication, therapy, or a holistic approach to navigating this new stage, know that help is available and help doesn’t make you weak. As a medication-taking, therapy-going, yoga-loving mom who loses her mind without these tools and resources… you’re in good company and no one wins a trophy for not needing help.